Genetic Mutations In Father’s Sperm Can Predict Children’s Autism Risk
There’s no question that autism can be traced to a combination of genetic and environmental factors. One genetic contributor in particular has in recent years intrigued scientists studying autism: DNA mutations originating in fathers’ sperm.
How AI Is Helping Diagnose Rare Genetic Diseases
Ten Children’s Hospitals Unite to Change Pediatric Care Through Genomic Medicine
Rady Children’s among founding members of innovative consortium SIOUX FALLS, S.D. — Nov. 5, 2019— Three more hospitals have signed on to rapidly integrate genetics and genomics into primary and specialty pediatric care through an innovative consortium with Sanford Health. Rady Children’s Hospital and Rady Children’s Institute for Genomic Medicine are founding members of the […]
Medical Marvels: Patients Get New Lives Through Physician Innovation

Maverick Coltrin was 6 days old and very, very sick. His parents were growing increasingly alarmed, first over his reluctance to eat, then jaundice and spasms. After Maverick stopped eating entirely, they raced him to the emergency room at Rady Children’s Hospital in San Diego.
Rady Children’s Institute for Genomic Medicine Receives $3 Million Grant to Investigate the Role Genes Play in Heart Muscle Disease
Four-year National Institutes of Health Grant to Focus on Cardiomyopathy Research SAN DIEGO – Sept. 27, 2019 – The National Institutes of Health has awarded Rady Children’s Institute for Genomic Medicine (RCIGM) a four year, $3,049,054 grant to investigate how genetic interactions may influence cardiomyopathy (CM), a devastating heart disease that affects millions in the […]
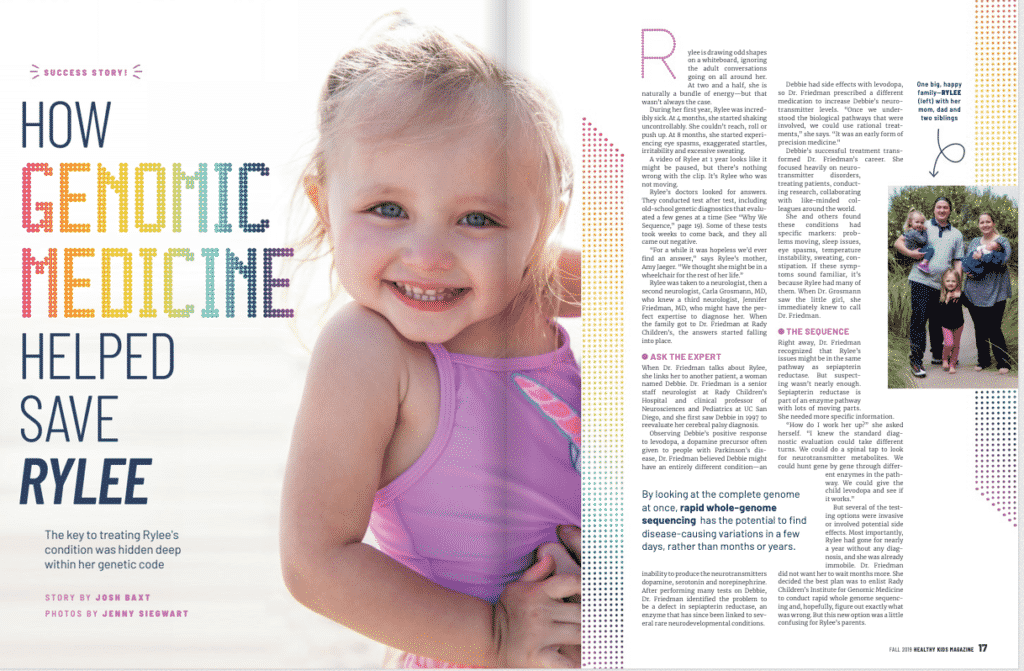
How Genomic Medicine Helped Save Rylee
Growing Up San Diego: Project Baby Bear is first of its kind in U.S.

NIH Newborn Sequencing Projects’ Lessons, Next Steps Highlighted at Meeting

As researchers wrap up four projects funded by the National Institute’s of Health in 2013 to investigate the use of sequencing in newborns, there seems to be clarity that sequencing is a great tool for helping to quickly diagnose acutely ill newborns but that it might not be quite ready to replace standard newborn screening tests […]
New Research Award Supports Early Career Investigator of Childhood Digestive Diseases
Funded 3-year appointment at Rady Children’s Institute for Genomic Medicine June 17, 2019—San Diego – A new research scholar position at Rady Children’s Institute of Genomics Medicine (RCIGM) has been awarded to a talented young investigator who is pursuing a career using genomics to enhance understanding of pediatric digestive diseases. Amy Hemperly, DO, is the […]
Rady Children’s Institute for Genomic Medicine Uses Artificial Intelligence to Diagnose Genetic Diseases
April 24, 2019–Researchers at Rady Children’s Institute for Genomic Medicine (RCIGM) have utilized automated machine-learning and clinical natural language processing (CNLP) to diagnose rare genetic diseases in record time. This new method is speeding answers to physicians caring for infants in intensive care and opening the door to increased use of genome sequencing as a […]